It’s easy to overlook how everyday habits impact your heels—until each step starts to sting. That tight stretch from your bed to the coffee machine becomes a painful reminder something isn’t right. A plantar fasciitis specialist can spot these habits quickly and guide you toward changes that don’t just treat pain, but prevent it from taking over again.
Incorporating Daily Calf Stretches to Alleviate Heel Pain
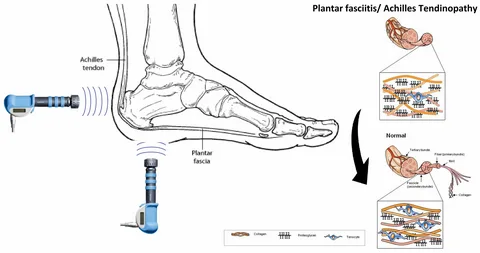
Stretching may seem basic, but to a plantar fasciitis specialist, it’s one of the first moves that can loosen up a tight fascia and reduce morning heel pain. Tight calf muscles put extra pull on the plantar fascia, the thick band of tissue that runs along the bottom of your foot. A quick set of calf stretches in the morning and evening helps ease this tension and can significantly reduce pressure on the heel where pain tends to flare up the most.
A common recommendation is the wall push stretch or using a towel for seated calf pulls. These movements keep the Achilles tendon and calf muscles limber, so your fascia isn’t overstretched with every step. The key is doing them consistently—every single day. Most plantar fasciitis doctors agree that daily flexibility work helps prevent microtears in the fascia from worsening, especially during busy routines.
Transitioning to Supportive Footwear to Ease Plantar Strain
What’s under your feet has a lot to do with what’s happening inside your heels. Swapping out flat shoes or worn-out sneakers for footwear with arch support and cushioned soles is one of the fastest ways to reduce strain on the plantar fascia. This shift gives your foot the structure it needs to distribute weight evenly, keeping pressure off inflamed areas.
Many people suffering from plantar fasciitis don’t realize their shoe choices are making the problem worse. A plantar fasciitis doctor will often check your footwear before anything else. Look for firm heel counters, ample arch support, and shock-absorbing midsoles. Even at home, ditching barefoot walking for supportive slippers or house shoes can make a big difference. Shoes are your foundation—make sure they’re doing their job.
Reducing High-Impact Exercises to Minimize Tissue Stress
High-impact activities like running, jumping, or fast-paced aerobics put repetitive force on your feet, which spells trouble for an already stressed fascia. A plantar fasciitis specialist often recommends pressing pause on these types of workouts—at least temporarily. The goal isn’t to stop moving but to shift toward low-impact options that let the fascia recover without losing overall fitness.
Consider biking, rowing, or pool workouts as effective substitutes while healing. These still raise your heart rate but eliminate the pounding force that aggravates heel pain. Giving your plantar fascia a break from constant micro-trauma is essential, especially if symptoms have persisted for weeks. Later, once the pain eases, a gradual return with proper footwear and pacing is usually safe.
Adjusting Sleep Habits with Night Splints for Fascia Recovery
It’s often overlooked, but how your feet rest at night affects how they feel in the morning. During sleep, the foot naturally points downward, keeping the plantar fascia shortened. Night splints help hold your foot in a neutral or slightly flexed position, allowing the fascia to stay elongated and gently stretch overnight.
A plantar fasciitis specialist may suggest these splints to reduce the stabbing pain that greets you in the morning. The idea isn’t to immobilize, but to maintain a gentle stretch while you sleep. Over time, this helps reduce stiffness and inflammation. It’s a passive fix that works while you rest, and many people notice smoother mornings within just a few weeks.
Adopting Anti-Inflammatory Nutrition to Reduce Heel Inflammation
What you put on your plate matters just as much as what you put on your feet. Inflammation plays a key role in plantar fasciitis, and food can either fan the flames or help extinguish them. A plantar fasciitis doctor might recommend leaning into anti-inflammatory eating—think omega-3 rich fish, leafy greens, berries, turmeric, and whole grains.
Avoiding foods that trigger inflammation, like processed sugars, refined carbs, and excess saturated fats, is just as important. Chronic heel pain is often tied to systemic inflammation, not just local irritation. A few mindful changes in your meals can complement physical therapy and foot care, creating a full-body response to heel pain that starts from the inside out.
Practicing Targeted Foot Strengthening to Prevent Fascia Injury
The foot contains dozens of small muscles that are easy to ignore until they start breaking down. Targeted strengthening, especially for the arch and intrinsic foot muscles, gives your fascia the support it needs. A plantar fasciitis specialist may suggest exercises like toe curls, marble pickups, or towel scrunches that activate and rebuild these key stabilizers.
Strengthening doesn’t just relieve pain—it helps prevent future injury. Over time, stronger foot muscles reduce the workload on the plantar fascia by absorbing more impact and improving overall foot mechanics. Doing these exercises for just 10 minutes a day can be a game-changer, especially when combined with stretching and supportive footwear.
Scheduling Regular Activity Breaks to Avoid Heel Overuse
Standing or walking for hours without rest can slowly wear down your plantar fascia, even if you’re wearing the best shoes in the world. A plantar fasciitis specialist will often emphasize the importance of pacing your day with built-in breaks. It’s not about doing less—it’s about doing smarter.
Breaks allow the fascia to recover and prevent the tissue from being overstretched repeatedly. Sitting for a few minutes every hour or doing quick stretch breaks can protect against flare-ups, especially in jobs that require prolonged standing. If you feel pain creeping in, that’s your cue to pause, reset, and give your feet the break they deserve. Regular breaks aren’t a luxury—they’re a recovery strategy.